What is Diabetes?
Diabetes is a serious condition where your blood glucose level is too high. It can happen when your body doesn’t produce enough insulin or the insulin it produces isn’t effective. Or, when your body can’t produce any insulin at all.
- We estimate that more than 5.8 million people in the UK are living with diabetes, which is an all-time high.
- Data shows that almost 4.6 million people in the UK live with diabetes diagnoses.
- Additionally, nearly 1.3 million people could be living with type 2 diabetes who are yet to be diagnosed.
There are two main types of diabetes: type 1 and type 2.
When you’ve got type 1 diabetes, you can’t make any insulin at all. If you’ve got type 2 diabetes, which is the most common, it’s a bit different. The insulin you make either can’t work effectively, or you can’t produce enough of it. They’re different conditions, but they’re both serious.
In all types of diabetes, glucose can’t get into your cells properly, so it begins to build up in your blood. And too much glucose in your blood causes a lot of different problems.

Symptoms of Diabetes
The symptoms can depend on the type of diabetes you have. But the common symptoms of diabetes include:
- Going to the toilet a lot, especially at night
- Being really thirsty
- Feeling more tired than usual
- Losing weight without trying to
- Genital itching or thrush
- Cuts and wounds take longer to heal
- Blurred vision
How is Diabetes diagnosed?
Diabetes is diagnosed from a blood test. If there are no obvious symptoms it can go undiagnosed.
Early diagnosis helps prevent diabetes complications.

Treatment for Diabetes
Treatment is about trying to keep blood sugars within a target range. Being as active as possible, eating healthily and going for regular health checks will help you do this. Some people will also need to take insulin or other medication and check their blood sugars regularly.
Lots of things can affect blood sugars, so it can be tricky to balance. But it’s possible to lead a full life. It’s about being in tune with your body and learning what works for you.
8 Care Processes
There are 8 care processes that are recommended to be completed annually; these care processes support you in self-managing your Diabetes and to reduce risk of complications.
- HbA1c (blood test)
- Blood pressure
- Cholesterol
- Kidney function
- Microalbumin (Urine)
- Foot checks
- BMI
- Weight
Diabetes remission
Type 2 Diabetes can be preventable, and for some, can be put into remission. This means your blood sugar levels are healthy without taking any medication.
For many people, this can be life-changing. That’s why Diabetes UK have put together guidance and advice for those of you who want to know more about diabetes remission.
For more information:
- Diabetes UK Midlands and East of England | Diabetes UK
- Diabetes UK Helpline | Diabetes UK
- Landing Page | Diabetes UK Learning Zone – free online learning modules for people with diabetes.
What is Pre-Diabetes
Some people may have a blood sugar level that is higher than usual, but not high enough to be diagnosed with type 2 diabetes. This is called prediabetes and means you’re at risk of developing type 2 diabetes.
You are unlikely to be experiencing any symptoms with prediabetes.
Pre-diabetes is also sometimes called borderline diabetes. Higher than normal blood sugar levels can be detected via blood tests.
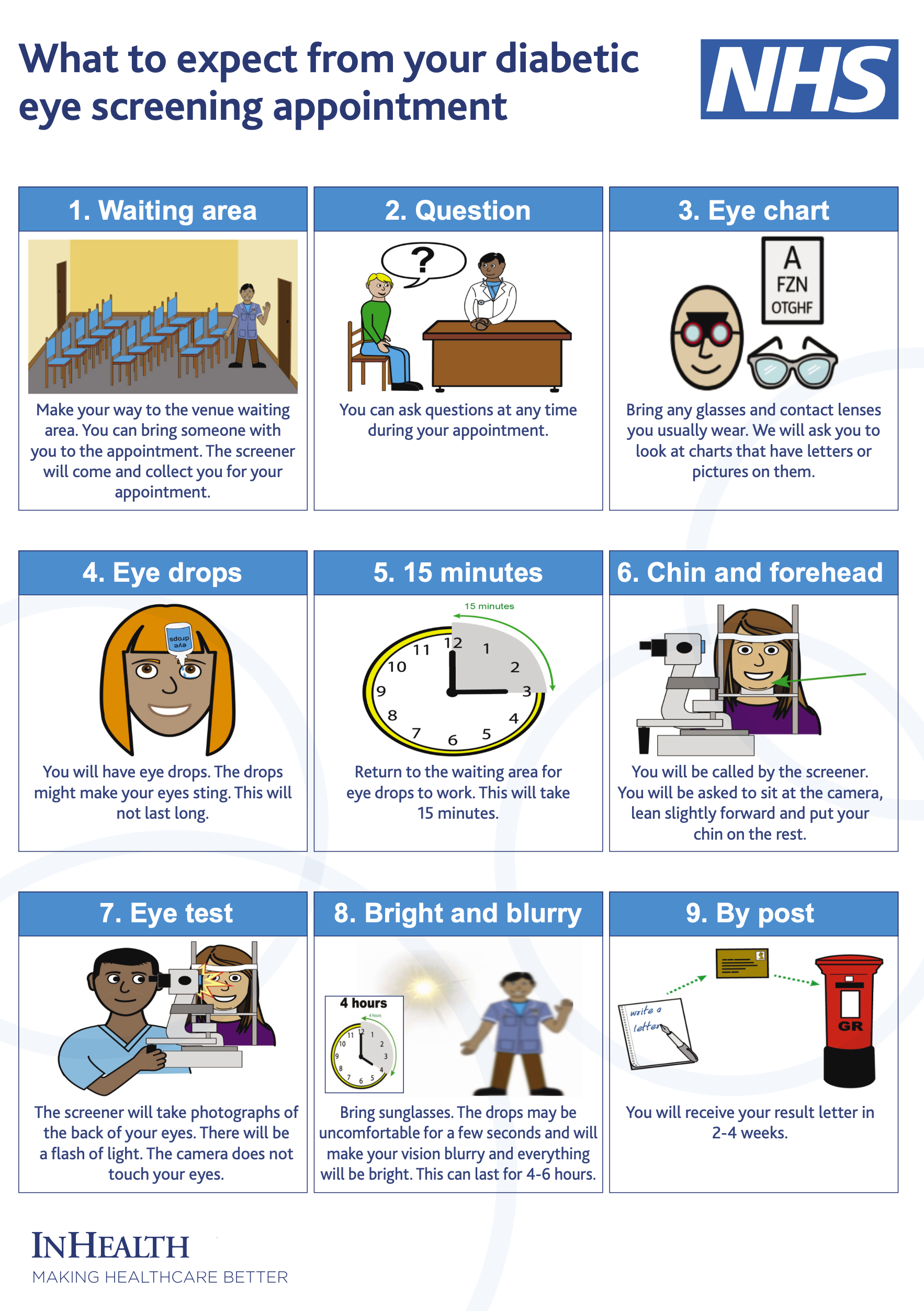
Eye screening information

Oviva
Desmond
The National Institute for Institute for Health and Care excellence (NICE) states DESMOND structured education is an integral part of diabetes care.
Those diagnosed with Type 2 Diabetes are encouraged to attend a free DESMOND one day course to invest in their health.
DESMOND provides understanding and equips the individual to manage their diabetes and prevent developing complications of Type2 diabetes.
NHS Talking Therapies
The CPFT LTC Talking Therapies is part of a national programme to support people with symptoms of anxiety, stress, low mood and depression associated with a long term physical health condition such as diabetes.
Talking Therapies offers to help people to self-manage their long term condition by reducing anxiety and depression, evidence based/NICE recommended treatment e.g. CBT & Mindfulness.
Face to face appointments, telephone appointments and on-line options are available.
How can I refer myself?
We recommend referral in the first instance via the web page:
Alternatively, email our self-referral team at SPAtalkingtherapies@cpft.nhs.uk Or call on the number below and they will guide you through the process. Let them know if you have a long-term physical health condition.
0300 300 0055 – The line is open 9am to 5pm, Mon to Fri.
Active Lifestyles & The Undefeatables
The Undefeatables
HDC Active Lifestyles offer a discounted membership for a period of 9-months to anyone with a diagnosis of Pre-Diabetes/ Diabetes.
The offer includes activities such as off-peak court hire, indoor cycling, gym sessions, fitness classes and swimming, amongst other targeted activities delivered across One Leisure.
The benefits of being active
Moving more can:
- Help you look after your blood pressure, because high blood pressure means you are more at risk of a range of health conditions, including diabetes complications
- Help to improve cholesterol (blood fats) to help protect against problems like heart disease
- Help you lose weight if you need to and keep the weight off after you’ve lost it
- Give you energy and help you sleep
- Help your joints and flexibility
- Help your mind as well as your body – exercise releases endorphins, which you could think of as happy hormones. Being active is proven to reduce stress levels and improve low mood
- Help people with type 2 diabetes improve their HbA1c. In some cases, this can help people with the condition go into remission
- Enables those with type 2 diabetes increase their insulin sensitivity
It is important to remember that being active is even more beneficial if you are also making healthier food choices, not smoking and getting enough sleep.
For more information or to apply visit: www.huntingdonshire.gov.uk/undefeat
